Aortic Disease
Aortic Aneurysm
 An aneurysm is an area of abnormal dilation or enlargement of an artery,
due to a weakening of its wall. The cause of this weakening is an abnormality
of the structural proteins that make up the vessel wall. This abnormality
can be due to a faulty gene, causing a defect in a structural protein
(see below). Environmental factors can also affect the structural proteins
of the vessel wall and cause aneurysm. The most well known of these is
cigarette smoking, which has long been understood to have a strong causative
association with abdominal aortic aneurysm. Atherosclerosis, or hardening
of the arteries, also has some degree of association with aneurysmal disease.
Given that structural proteins in all the arteries are involved, aneurysms
often occur in more than one location within a given individual. For example,
10% of individuals with a popliteal artery (behind the knee) or an iliac
artery (in the pelvis) aneurysm also have an abdominal aortic aneurysm.
An aneurysm is an area of abnormal dilation or enlargement of an artery,
due to a weakening of its wall. The cause of this weakening is an abnormality
of the structural proteins that make up the vessel wall. This abnormality
can be due to a faulty gene, causing a defect in a structural protein
(see below). Environmental factors can also affect the structural proteins
of the vessel wall and cause aneurysm. The most well known of these is
cigarette smoking, which has long been understood to have a strong causative
association with abdominal aortic aneurysm. Atherosclerosis, or hardening
of the arteries, also has some degree of association with aneurysmal disease.
Given that structural proteins in all the arteries are involved, aneurysms
often occur in more than one location within a given individual. For example,
10% of individuals with a popliteal artery (behind the knee) or an iliac
artery (in the pelvis) aneurysm also have an abdominal aortic aneurysm.
Aneurysms can occur in any artery at any location: arteries in the brain,
thoracic aorta, abdominal aorta, hepatic (liver) artery, splenic (spleen)
artery, renal (kidney) artery, mesenteric (intestinal) arteries, iliac
arteries, femoral (thigh) artery, popliteal artery. Many of these arteries
are situated deep in the body, such that an aneurysm can form in the artery
and grow to a large size, yet still remain undetected. Indeed, most aneursyms
are found by accident, when a patient undergoes an x-ray, ultrasound,
CT, or MRI scan for an unrelated problem.
Why Are Aneurysms Dangerous?
Aneurysms can be dangerous in two different ways:
- The aneurysm can rupture, causing severe or life-threatening bleeding.
- The aneurysm can develop clots in its wall, which can subsequently break
off and travel to different organs.
Aneurysms can grow quite large before they rupture. When an aneurysm ruptures,
the result is catastrophic and severe life-threatening bleeding ensues.
In general, when an aneurysm reaches twice the size (2X diameter) of the
associated native artery, the risk of rupture becomes substantial. Until
the aneurysm reaches 2X diameter, it is safe to just watch it closely
(“watchful waiting”) with serial ultrasound or CT imaging
studies. Once the 2X diameter is reached, however, repair of the aneurysm
should be strongly considered. Of course, the decision to perform surgical
or endovascular repair depends on the risk of a given surgical procedure,
weighed against the risk of aneurysm rupture by continued watchful waiting.
In contrast to the size factor involved in aneurysm rupture, aneurysms
can form clots at any size. The clots form in an aneurysm because of the
blood flow patterns in an aneurysm sac, such that there are regions where
flow eddies exist and other regions where blood flow is slow or almost
stand-still. The blood forms clots in these regions. These clots can then
break off and travel to branch blood vessels distal to the aneurysm and
block blood flow in these vessels, causing the organ tissue supplied by
these vessels to become damaged and die. This condition can be life- or
limb-threatening.
The Genetics of Aneurysms
Some rare genetic diseases are associated with aneurysms. Ehlers-Danlos
syndrome is a disease associated with abnormalities of the connective
tissue. It is caused by a defect in the gene for collagen, a central protein
in connective tissue, including the wall of blood vessels. Patients with
this disorder have loose skin, frequent bruising, hyper-flexible joints,
mitral valve prolapse or other cardiac valve abnormalities, and aortic
aneurysm (typically of the thoracic aorta). Marfan syndrome is another
genetic abnormality associated with aortic aneurysm. It is caused by a
defect in the gene for fibrillin, another connective tissue structural
protein. Marfan syndrome patients are typically of tall and slender build,
have disproportionately long arms, legs, fingers, and toes, a breastbone
that protrudes outward or inward, a high arched palate, abnormalities
of the ocular lens, a curved spine, lung abnormalities such as propensity
for a collapsed lung, cardiac valve abnormalities, and aortic aneurysm
or dissection. Aside from the above two named genetic diseases, a condition
of weakening of the arterial wall, known as “cystic medial necrosis,”
which has a strong familial factor, has been identified to be associated
with aortic aneurysm. There are likely multiple genes involved in the
formation of aortic aneurysm, which remain to be identified and understood.
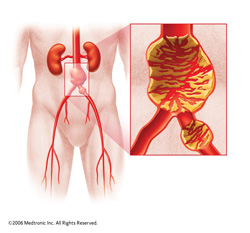
Abdominal Aortic Aneurysm
 Abdominal aortic aneurysm (AAA) is a serious condition in which the abdominal
aorta (below the diaphragm and above the groin) enlarges to a point at
which it ruptures or becomes at high risk of rupturing. This disease is
very common in smokers (90% of patients with AAA are smokers). AAA is
more common in men than in women, and is more common in patients with
atherosclerosis.
Abdominal aortic aneurysm (AAA) is a serious condition in which the abdominal
aorta (below the diaphragm and above the groin) enlarges to a point at
which it ruptures or becomes at high risk of rupturing. This disease is
very common in smokers (90% of patients with AAA are smokers). AAA is
more common in men than in women, and is more common in patients with
atherosclerosis.
AAA usually does not cause any symptoms. It is often discovered by chance,
when a patient has an abdominal ultrasound or abdominal CT for some other
unrelated problem. Thus, AAA is a “silent killer.” Its danger
lies in the fact that there are no symptoms, and the first sign of trouble
is usually when the aneurysm actually ruptures. This event almost always
results in death. Only 50% of AAA rupture patients reach the hospital
alive. Only 10% of AAA ruptures survive. Because of the high mortality
involved after an aneurysm rupture, the goal of AAA treatment is early
diagnosis and treatment, before rupture occurs. The operative risk for
an elective AAA surgical repair is 5 – 10%, compared to a mortality
risk of 50% once an AAA ruptures.
Because of the expense of screening programs, it is not economically feasible
to scan everyone for AAA, and screening is focused on those individuals
who are at high risk for AAA. Thus, targeted screening is the current
strategy, and individuals should be screened if they have a history of
heavy smoking, or a family history of aneurysms. In 2009, congress passed
the SAAAVE Act, which funds ultrasound screening for AAA as part of the
Welcome to Medicare Package--in individuals who turn 65 who have a history
of smoking or a family history of aneurysm.
Screening for AAA is principally done by abdominal ultrasound. This test
is fairly inexpensive, involves no radiation, takes about 20 min., and
is widely available in most medical offices and medical centers. The procedure
involves scanning the abdomen with ultrasound waves, and directly visualizing
and measuring the dimensions of the abdominal aorta. Other modalities
to image the abdominal aorta include CT or MRI scanning. These modalities
are much more expensive, not as widely available, involve an IV, and in
the case of CT, involve radiation to image the area of interest.
Abdominal aortic aneurysms grow slowly. They typically enlarge in diameter
by about 10% per year. Thus, an aneurysm that is currently 3.0 cm now
will grow to about 3.3 cm in one year. However, note that the larger an
aneurysm gets, the faster it will grow. An aneurysm that is 4.5 cm now
will likely be 5.0 cm in one year. The normal diameter of the abdominal
aorta is about 2.5 cm. In men, the rupture risk of an AAA becomes significant
when the aneurysm reaches about 5.0 cm, and this is the point at which
intervention should be considered. Women tend to have smaller aorta dimensions,
and intervention should be considered at an aortic diameter of 4.5 cm.
Aneurysms can be “fusiform” or “saccular” in shape.
A “fusiform” aneurysm is relatively symmetric, shaped much
like a blimp. Fusiform aneurysms tend to enlarge symmetrically and at
an even rate in all sections. In contrast, a “saccular” aneurysm
is asymmetric in shape, such as like a pear. Saccular aneurysms enlarge
asymmetrically, with some regions enlarging faster than others, and can
grow faster than fusiform aneurysms. Thus, saccular aneurysms should be
watched at more frequent intervals, and should be intervened upon at relatively
smaller sizes.
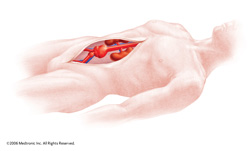
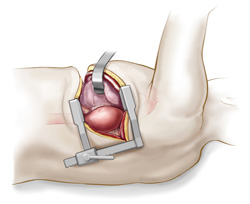
 There are two ways to repair AAA. The classic repair has been through open
surgery. In this procedure, the surgeon makes a laparotomy incision in
the abdomen. The aorta is then crossclamped and incised. The repair is
done by sewing a prosthetic tube graft into the region of diseased aorta.
Open repair of AAA is a major surgical procedure, usually involving several
days in the intensive care unit, and about a week total time in hospital.
In patients with cardiac or lung problems, open AAA repair carries with
it a high risk of peri-procedure heart attack or lung complications. Until
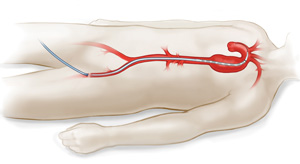
recently, most AAA procedures were done with open surgery. In recent years,
a new endovascular treatment of AAA has emerged--EndoVascular Aortic Repair
(EVAR), in which the aorta is treated “from the inside” by
placing a stent within it. The stent is covered with a synthetic nonporous
material, such that after the stent is placed inside the aorta, the aneurysm
outside the stent becomes excluded and eventually clots off.
There are two ways to repair AAA. The classic repair has been through open
surgery. In this procedure, the surgeon makes a laparotomy incision in
the abdomen. The aorta is then crossclamped and incised. The repair is
done by sewing a prosthetic tube graft into the region of diseased aorta.
Open repair of AAA is a major surgical procedure, usually involving several
days in the intensive care unit, and about a week total time in hospital.
In patients with cardiac or lung problems, open AAA repair carries with
it a high risk of peri-procedure heart attack or lung complications. Until
recently, most AAA procedures were done with open surgery. In recent years,
a new endovascular treatment of AAA has emerged--EndoVascular Aortic Repair
(EVAR), in which the aorta is treated “from the inside” by
placing a stent within it. The stent is covered with a synthetic nonporous
material, such that after the stent is placed inside the aorta, the aneurysm
outside the stent becomes excluded and eventually clots off.
 The stent is inserted through the femoral artery by making an incision
in the groin, thus avoiding the abdominal incision and dramatically reducing
the recovery time. In most cases, the hospitalization is only 2 days.
In some centers, even the groin incision is done using “pinhole
incision” techniques, thus reducing the size of the incision wound--and
its inherent infection risks--even further. In addition, the associated
cardiac risks of open surgery are avoided. Currently in the US, about
75% of AAA repairs are done endovascularly. The choice of endovascular
versus surgical repair is based primarily on the anatomy of the iliac
and femoral vessels, through which the stent must be inserted, and the
precise location of the aneurysm and its relation to nearby branch vessels.
The stent is inserted through the femoral artery by making an incision
in the groin, thus avoiding the abdominal incision and dramatically reducing
the recovery time. In most cases, the hospitalization is only 2 days.
In some centers, even the groin incision is done using “pinhole
incision” techniques, thus reducing the size of the incision wound--and
its inherent infection risks--even further. In addition, the associated
cardiac risks of open surgery are avoided. Currently in the US, about
75% of AAA repairs are done endovascularly. The choice of endovascular
versus surgical repair is based primarily on the anatomy of the iliac
and femoral vessels, through which the stent must be inserted, and the
precise location of the aneurysm and its relation to nearby branch vessels.
Thoracic Aortic Aneurysm
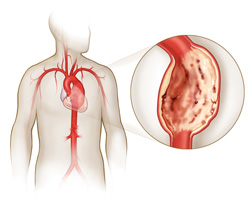 Thoracic aortic aneurysm (TAA) is a relatively rare disease, much less
common than AAA. The factors that cause TAA involve structural weakening
of the aortic wall, and genetic defects are a prominent factor in TAA.
However, there is not a strong association with smoking and TAA, as there
is in the case of AAA. TAA is more common in men than in women. TAA sometimes
develops in association with another disorder of the aorta--Aortic Dissection.
In aortic dissection, a tear occurs in the inner lining of the aorta.
This in itself is a dangerous event and can be life-threatening. After
a dissection occurs, the aortic wall begins to heal itself, but because
the wall is weakened, it can, over the ensuing years, develop into an aneurysm.
Thoracic aortic aneurysm (TAA) is a relatively rare disease, much less
common than AAA. The factors that cause TAA involve structural weakening
of the aortic wall, and genetic defects are a prominent factor in TAA.
However, there is not a strong association with smoking and TAA, as there
is in the case of AAA. TAA is more common in men than in women. TAA sometimes
develops in association with another disorder of the aorta--Aortic Dissection.
In aortic dissection, a tear occurs in the inner lining of the aorta.
This in itself is a dangerous event and can be life-threatening. After
a dissection occurs, the aortic wall begins to heal itself, but because
the wall is weakened, it can, over the ensuing years, develop into an aneurysm.
TAA is dangerous because there are usually no symptoms and the aneurysm
continues to grow silently. Many times, the diagnosis is made by accident
when the patient undergoes a chest x-ray or CT for an unrelated illness.
Rarely, the aneurysm can cause symptoms of chest pain. If the aneurysm
impinges on the nearby structures, such as the laryngeal nerve or the
trachea or esophagus, symptoms of hoarseness or wheezing or difficulty
swallowing can occur.
The risk of TAA rupture becomes significant when the aneurysm reaches 6.0
cm in the ascending aorta or 7.0 cm in the descending aorta. Fortunately,
thoracic aneurysms grow very slowly, on the order of millimeters per year.
Monitoring of TAA size can only accurately be done by CT or MRI. Chest
x-ray or ultrasound cannot accurately assess TAA size.
 Open surgical repair of TAA is a major procedure, with significant risk
involved. In addition to the usual risks involved in aneurysm surgery,
there is a risk for spinal cord damage and paralysis after TAA repair.
This is because branch arteries from the thoracic aorta supply blood to
the spinal cord, and these can be injured during surgery of the aorta.
Open surgical repair of TAA is a major procedure, with significant risk
involved. In addition to the usual risks involved in aneurysm surgery,
there is a risk for spinal cord damage and paralysis after TAA repair.
This is because branch arteries from the thoracic aorta supply blood to
the spinal cord, and these can be injured during surgery of the aorta.
Endovascular repair of the thoracic aorta is a technique in which the aorta
is repaired by placement of a stent. The stent, covered with a non-porous
fabric material, is inserted through the groin and implanted inside the
aorta. The aneurysm is excluded and eventually clots off. The procedure
is much safer than open surgical repair of the thoracic aorta and also
involves a lower risk of spinal cord injury and paralysis.