Interventional Treatment
 Cardiac Cath
Cardiac Cath
Cardiac catheterization, also known as coronary angiogram, or "heart
cath," is a procedure in which the coronary arteries and heart muscle
are directly imaged under x-ray using iodine contrast dye. Cardiac cath
is the "gold standard" for diagnosis of coronary disease. The
procedure is usually performed through the femoral artery in your groin
but is sometimes performed through the brachial artery on the inner aspect
of your elbow. During a cardiac cath, your cardiologist administers local
anesthesia to numb the groin, then inserts a thin, hollow catheter into
the femoral artery in the groin and advances it to the heart. Injection
of contrast through the catheter under x-ray allows visualization of the
coronary arteries. Blockages, or "stenoses" of the coronaries
can be identified in this manner. Cardiac cath takes about one hour and
can be done in an outpatient manner. However, if an angioplasty is performed
at the same time as a heart cath, the patient is usually admitted to the
hospital overnight for observation.
Pacemaker
A slow heart rhythm, or bradycardia, can be treated with a permanent pacemaker.
This sophisticated device is only about the size of a silver dollar coin
and is implanted beneath the skin in the upper chest. The procedure is
done under local anesthesia. The pacemaker lies dormant as long as the
heart is beating normally. However, if the heart should beat inappropriately
slowly, the pacemaker "kicks in" and paces the heart.
Coronary Angioplasty Stent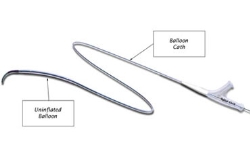
Coronary angiography, described above, is a diagnostic procedure during
which the coronary arteries are imaged in order to define their anatomy
and identify stenoses, or blockages, within the arteries. Coronary angioplasty,
or percutaneous transluminal coronary angioplasty (PTCA), is a therapeutic
procedure geared toward treating coronary stenosis or occlusion. During
this procedure, the cardiologist advances an angioplasty balloon into
the coronary artery and, under x-ray guidance, positions the balloon over
the site of the blockage, or stenosis. Inflation of the balloon stretches
the artery, compressing the plaque against the artery wall, thereby enlarging
the artery channel. While the balloon is inflated, it occludes the artery
channel and blood cannot pass. During this time, the patient may experience
chest discomfort, until the balloon is deflated. Following angioplasty,
the artery channel is enlarged. However, since the artery contains elastic
tissue, there is always some degree of "recoil" after the balloon
is deflated. Over the ensuing weeks, as the artery heals, the recoil process
may continue. In some cases (30-40%), severe recoil can cause "restenosis,"
or re narrowing of the arterial channel. This is a drawback to angioplasty.
Fortunately, a device known as a "stent" has been developed
that completely overcomes the recoil phenomenon.
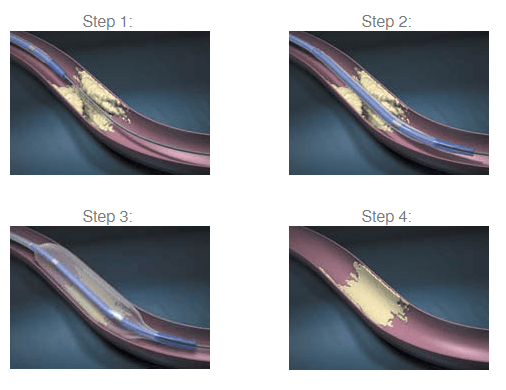
Coronary stents are designed to be placed into the coronary arteries that
lie on the surface of the heart and supply the heart with oxygen-fresh
blood. A stent is mounted on an angioplasty balloon in its collapsed state.
The stent/balloon assembly is then advanced into the coronary artery and
positioned over the site of the coronary lesion. When the balloon is inflated,
the stent becomes fully expanded and apposed against the coronary artery
wall, "tacking up" the atherosclerotic lesion and buttressing
the artery wall. The balloon is then removed but the stent remains in
the coronary artery (forever). As a result of advancing stent design,
more patients with more complex disease are candidates for stenting, which
reduces the number of coronary artery bypass graft surgeries.
Stenting has been an important advance in balloon angioplasty. Before
the introduction of stents, as many as half of all coronary arteries opened
with a balloon-tipped catheter narrowed once again after the procedure(restenosis).
In 2003, a major advancement in stenting was realized with the introduction
of a new generation of stents. These stents, call "drug-eluting"
stents, are covered with special drugs that reduced the restenosis rate
to its current low level. Today, drug-eluting stents comprise the majority
of stents in clinical use for coronary disease.
Following stenting, the patient is treated with aspirin in addition to
blood thinner, in order to prevent blood clotting at the site of the stent.
It is important for the patient to carefully follow their physician's
orders regarding these medications, as well as practice healthy lifestyle
behaviors, such as not smoking and lowering cholesterol levels. Stents
are not affected by metal detectors or most mechanical equipment.
Defribillator / AICD
 An automatic implantable cardiac defibrillator is a device capable of detecting
a dangerous heart rhythm and applying an electrical shock to the heart
in order to convert the rhythm back to normal. This device is implanted
under the skin under local anesthesia, much like a pacemaker, in patients
who have a predisposition to dangerous arrhythmias that could cause loss
of consciousness. Following implantation, the device is checked at regular
intervals several times a year, on an outpatient basis.
An automatic implantable cardiac defibrillator is a device capable of detecting
a dangerous heart rhythm and applying an electrical shock to the heart
in order to convert the rhythm back to normal. This device is implanted
under the skin under local anesthesia, much like a pacemaker, in patients
who have a predisposition to dangerous arrhythmias that could cause loss
of consciousness. Following implantation, the device is checked at regular
intervals several times a year, on an outpatient basis.
Electrophysiology Study
A study of the Heart's electrical system is know as an electrophysiology
test. During this test, wire electrode catheters are advanced through
a vein in the groin to various positions in the heart. The electrical
activity of the heart is then examined and the conduction properties of
the nerves in the heart are measured. The second part of this test involves
electrical stimulation of various parts of the heart in an attempt to
induce an abnormal heart rhythm. Identification of this abnormal rhythm
allows specific treatment to be tailored towards it. Electrophysiology
testing is usually performed on patients with symptoms of dizziness or
fainting. In some instances, a Holter monitor may pick up an abnormal
and potentially dangerous heart rhythm that is further investigated by
elecrophysiology study.
Tilt Table Test
An automatic implantable cardiac defibrillator is a device capable of detecting
a dangerous heart rhythm and applying an electrical shock to the heart
in order to convert the rhythm back to normal. This device is implanted
under the skin under local anesthesia, much like a pacemaker, in patients
who have a predisposition to dangerous arrhythmias that could cause loss
of consciousness. Following implantation, the device is checked at regular
intervals several times a year, on an outpatient basis.