Heart In Health & Disease
The Heart Muscle
The heart is a very specialized muscle consisting of four chambers: a right
and a left upper chamber (atrium) and a right and a left lower chamber
(ventricle). The atria are thin-walled reservoirs for blood and empty
directly into the thick walled, muscular lower chambers, which contract
and pump the blood out of the heart. The heart is really "two hearts
that beat as one." The left atrium and ventricle receive red, oxygenated
blood from the lungs and pump it to the body. The right atrium and ventricle
receive blue, de-oxygenated blood from the body and pump it to the lungs,
where the blue blood is oxygenated.
The arteries are blood vessels that carry blood away from the heart, whereas
veins carry blood back towards the heart. The heart muscle itself receives
blood supply from two arteries: the left coronary and right coronary artery.
"Coronary" means "crown" and the coronary arteries
get their name by the fact that they encircle the top portion of the heart
much like a crown. Specialized nerve cells in the heart generate and conduct
electrical impulses that initiate the heart beat and coordinate the timing
of contraction of the various chambers and allow the heart to beat in
an organized fashion. A heart beat cycle consists of systole, when the
heart is contracting and ejecting blood, and diastole, when the heart
is relaxing and filling with blood for the next contraction.
 Congestive Heart Failure
Congestive Heart Failure
The heart is a muscular pump. In health, the heart circulates blood through
the body by contracting vigorously in systole and ejecting blood into
the great vessels, then relaxing in diastole and allowing blood to fill
the ventricle in preparation for the next systolic contraction. The proper
function of the heart depends both on normal contraction in systole and
normal relaxation in diastole. Many disease states can weaken the heart
muscle and affect its ability to contract normally. Some of these diseases
include coronary atherosclerosis, heart attack, valvular heart disease,
severe hypertension, thyroid disease, alcoholism, drug abuse, chemotherapy
treatment, and viral infection. These disease states vary in mechanism,
but all lead to the final common result of a heart that is enlarged and
that weakly contracts. This is known as dilated cardiomyopathy, or enlarged
heart, and is the cause of congestive heart failure. In left-sided congestive
heart failure, a weakened left ventricle is unable to pump blood efficiently
to the body. As a result, the blood backs up in the lungs, causing symptoms
of shortness of breath. In right-sided congestive heart failure, a weakened
right ventricle results in blood backing up in the lower extremities and
causing leg swelling.
Improper relaxation of the left ventricle in diastole may also lead to
left-sided congestive heart failure by not allowing the blood returning
from the lungs to easily flow into the left ventricle. This is known as
diastolic dysfunction, and results in the lungs becoming congested with
blood. Congestive heart failure due to diastolic dysfunction frequently
is associated with chronic hypertension but also occurs in the absence
of hypertension as the normal heart ages.
Congestive heart failure is treated medically with digitalis, diuretics,
ACE inhibitors, nitrates, and beta blockers. If a reversible underlying
cause can be identified, more specific treatment is initiated. For example,
congestive heart failure due to coronary disease is treated by coronary
bypass or angioplasty.
In recent years, the area of congestive heart failure has itself become
a subspecialty within cardiology, and congestive heart failure clinics
are now open in many parts of the country.
Early symptoms of coronary artery disease include chest pain on exertion,
or "angina." As the coronary artery disease progresses, the
angina may occur with less and less exertion. This exertional angina (
also called stable angina) is significant with regards to symptoms but
is also significant because the presence of cholesterol plaque in the
coronary artery has the potential to cause myocardial infarction, or heart
attack. Under certain conditions, a coronary plaque may become unstable
and rupture. The various factors that lead to plaque rupture are not well
understood and are currently actively being investigated. Coronary plaque
rupture exposes the fatty contents of the plaque to the circulating blood,
leading to a blood clot that occludes the channel of the coronary artery
and prevents blood from flowing to the heart muscle. This results in "unstable
angina" and heart attack, which are characterized by angina at rest.
Stable exertional angina is treated with a three-tiered approach of risk
factor modification, medications, and coronary revascularization. Risk
factor modification includes weight loss, adoption of a diet low in saturated
fat, cessation of smoking, and initiation of an exercise program. These
measures are aimed at reducing the coronary risk factors. Medications
include aspirin, beta blockers, ACE inhibitors, and cholesterol-lowering
drugs, all of which have been shown to reduce the risk of heart attack.
Treatment of hypertension is done using a variety of antihypertensive
agents nitrates are prescribed for controlling symptoms of angina. Coronary
revascularization--with angioplasty or coronary artery bypass surgery--is
performed in selected patients for relief of symptoms and, in some patients,
for survival benefit.
Coronary Arteries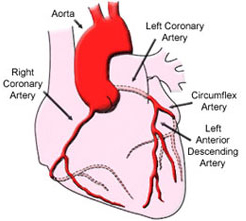
The heart receives its blood supply from two coronary arteries: left coronary
artery and right coronary artery, which are the first arteries to branch
from the aorta. These principal arteries branch many times and finally
become capillaries that supply the heart muscle. The left coronary (left
main) branches into the left anterior descending artery, which supplies
the anterior, or "front wall" of the left ventricle, and the
circumflex, which supplies the lateral, or "side wall" of the
left ventricle. The right coronary supplies the right ventricle as well
as the posterior and inferior walls, or "back side," of the
left ventricle. Blood flow to the heart muscle occurs during diastole,
or between contractions, when the heart muscle is resting.
Coronary Artery Disease
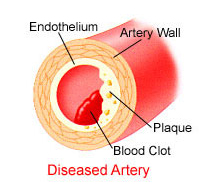
The coronary arteries, can become diseased, a condition known as coronary
insufficiency. Various conditions--such as elevated serum cholesterol,
hypertension, diabetes, cigarette smoking--cause cholesterol deposits
to accumulate in the inner lining of the coronary arteries, a process
called atherosclerosis. Atherosclerosis is a slow process, occurring over
decades, and results in a gradual narrowing of the channel of the coronary
artery as well as diminished arterial capacity to dilate under work load
conditions. The result is a compromise to the blood flow to the heart
muscle. This compromise may not manifest when the body is at rest but
becomes much more significant under work conditions.
Even under "normal" conditions, the workload demands on the heart
vary significantly. When the body is at rest, the heart's oxygen demand
is relatively low and the coronaries supply enough blood for baseline
heart function. During exercise, the body's blood demands rise greatly
and the heart must increase it's output of blood to meet these needs.
In order to do this, the heart itself demands greater blood supply. In
a healthy heart under work load conditions, the coronary arteries have
a tremendous capacity to dilate, increasing by several fold their delivery
of blood to the working heart muscle. However, when the coronary arteries
become diseased, they lose the capacity to dilate and increase delivery
of blood to meet the body's needs. The result is coronary insufficiency.
 Heart Valves
Heart Valves
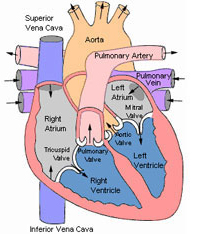
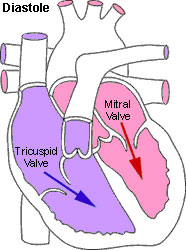
Blood flows through the heart in one direction. This unidirectional flow
is made possible by the action of four valves inside the heart: tricuspid,
mitral, aortic, and pulmonic. The tricuspid valve is located between the
right atrium and right ventricle and opens during diastole, allowing blood
to pass from right atrium to right ventricle. When the right ventricle
contracts in systole, the higher pressure in the right ventricle forces
the tricuspid valve to close and the pulmonic valve to open. Since blood
cannot pass backwards through the closed tricuspid valve, it is forced
out of the right ventricle through the open pulmonic valve into the pulmonary
artery and on to the lungs for oxygenation. The oxygenated blood returns
to the heart from the lungs via the pulmonary vein, which empties into
the left atrium. Separating the left atrium from the left ventricle is
the mitral valve. During diastole, the mitral valve opens and blood from
the left atrium fills the left ventricle. When the left ventricle contracts
during systole, the mitral valve closes, the aortic valve opens, and blood
is vigorously ejected through the aortic valve and into the aorta, which
carries oxygenated blood to the body. The "lub-dub" sound that
one hears when listening through a stethoscope is actually the sound of
moving blood striking against the valves that "slam" shut as
the heart contracts and relaxes. A heart murmur is an extra sound that
may be heard if there is turbulence of blood flow across a valve.
Valvular Heart Disease
In a normal, healthy heart, the blood flows freely through the valves when
they are open but cannot leak through them when the valves are closed.
Heart valves can become diseased, however, leading either to improper
opening or improper closing of the valve.
In some disease states, the normal valve elasticity and compliance is lost
over time and the valve becomes stiff, immobile, and unable to open completely,
causing an obstruction to the free flow of blood (stenosis). Examples
of diseases in which this occurs are mitral valve stenosis ensuing from
rheumatic heart disease and aortic stenosis due to calcification and thickening
of the aortic valve.
Alternatively, valves may close improperly and become leaky (regurgitant).
This may occur because the heart has become enlarged or because the valve
tissue has become degenerative for various reasons (valve infection, severe
mitral valve prolapse, phen-fen use). Both valvular stenosis and regurgitation
may cause an audible heart murmur.
Typical symptoms of valvular disease consist of shortness of breath and
fatigue. In severe cases, dizziness or fainting may occur. Valvular disease
may also lead to heart rhythm disturbances.
Valvular disease is quantified and graded as mild, moderate, or severe.
Mild or moderate valve stenosis or regurgitation are usually treated with
medications. However, severe valvular stenosis or regurgitation requires
surgical treatment. This involves open heart surgery with repair or removal
of the diseased valve and replacement with a prosthetic valve. Two main
types of prosthetic valves are currently used: mechanical tilting disc
valves (made of metal and plastic) and tissue bioprosthetic valves (made
of porcine or bovine tissue). Mechanical valves require that the patient
be placed on lifelong blood thinner (warfarin), whereas bioprosthetic
valves do not. However, mechanical valves in general are more durable
and less likely to degenerate with time.
Patients with significant valvular disease or prosthetic valves are instructed
to take prophylactic antibiotics prior to having any dental work, in order
to prevent infection of the diseased/prosthetic valve.
 Electronic Conduction System
Electronic Conduction System
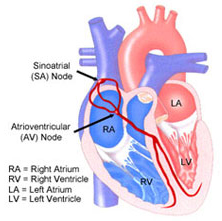
The organized beating of the heart takes place because of the heart's
sophisticated conduction system, or "electrical wiring." The
electrical impulse for a heartbeat begins in the sinoatrial (SA) node,
a specialized group of pacemaker cells located in the right atrium which
initiate a regular, clockwork-like series of electrical impulses that
ultimately lead to a heartbeat. The SA node is responsive to the physiologic
needs of the body and can increase or decrease its rate of firing accordingly.
The electrical impulse that riginates in the SA node travels rapidly via
nerve fibers through both atria to the atrioventricular (AV) node. As
the impulse passes through the atria, it is dispersed to the muscle tissue
in the atria and stimulates both atria to contract simultaneously and
empty their contents into their respective ventricles. The AV node is
like a "grand central station" of nerve fibers, and here the
electrical impulse is slowed down and organized. This allows time for
blood to pass from atria to the ventricles. From the AV node the impulse
passes to the nerve bundle of His and Purkinjie fibers (named after the
scientists who discovered them). These nerve fibers are like a system
of "freeways" that rapidly carry the impulse and distribute
it to both ventricles. The impulse reaches various regions of the ventricle
in a specific order that leads to a choreographed ventricular contraction,
such that contraction begins at the bottom (apex) of the heart and ends
at the top (base) of the heart. This results in efficient ejection of
blood out of the heart.
Arrhythmia
Disturbances in the sophisticated electrical wiring of the heart lead to
abnormalities of the heart rhythm, or arrhythmia. The study and treatment
of these arrhythmias is called electrophysiology. Arrhythmias can be divided
into bradycardia (slow heart beat) and tachycardia (fast heart beat).
Bradycardia usually result from degenerative disease of the conduction
nerves and nerve centers in the heart, such as the sinus node, AV node,
and bundle of His. For example, the sinus node may fire too slowly or
not fire at all, causing sinus arrest. In this setting, one of the backup
pacemaker centers of the heart takes over, usually at a very slow heart
rate. Alternatively, the AV node may conduct too slowly or not at all,
causing a breakdown in communication between the atria and ventricles,
or AV dissociation. Severe disease in the Bundle of His may also cause
AV dissociation. Some bradycardia may also result from high dose of medications,
such as beta blockers. Bradycardia may cause symptoms such as weakness,
dizziness, or fainting spells. Severe bradycardia are treated with a pacemaker.
Tachycardia are characterized by an erratic, rapid beating of the heart
that overrides the normal SA node pacemaker. Tachycardia that have their
origin in the atria are called atrial tachycardia. These include atrial
fibrillation, atrial flutter, and atrial tachycardia.
Atrial fibrillation is a very common arrhythmia characterized by a very
rapid and irregular beating of the heart. This arrhythmia is usually treated
with digoxin or a beta blocker for control of the heart rate. Other antyrrhythmic
drugs, such as stall, disopyramide, or amiodarone may be added to suppress
the fibrillation rhythm itself. In some cases, electrical shock can be
used to convert the patient back to sinus rhythm. Since atrial fibrillation
may lead to the formation of blood clots in the heart, patients with atrial
fibrillation are usually treated with coumadin, a potent blood thinner,
to prevent the occurrence of stroke.
Atrial flutter and atrial tachycardia typically cause symptoms of palpitations
or lightheadedness.
Tachycardias that originate in the ventricles, termed ventricular tachycardias,
are usually more dangerous in that they may cause severe drops in blood
pressure, leading to loss of consciousness. Some of these arrhythmias
can be controlled with medications. However, some severe tachycardias
cause repeated lapses of consciousness and are life-threatening. These
are treated with an automatic implantable cardiac defibrillator (AICD),
a device implanted under the skin that detects a dangerous tachycardia
and terminates it with an electrical shock. Some difficult-to-treat tachycardias
that do not respond to medicine may be ablated by radio-frequency catheter
ablation therapy, which is done through a catheter in the groin.